

described substantial, generalised cognitive impairment in schizophrenia across multiple domains. Further studies are required.Ĭognitive impairment is a core feature of schizophrenia 1 that is less amenable to treatment than its two other core features: psychotic symptoms (especially) and negative symptoms. There was a statistically significant difference between participants' performance on the MMSE and MoCA tests (p = 0.000008).ĬONCLUSION: Compared to the MMSE, the MoCA may be a more useful instrument to detect cognitive impairment in patients with schizophrenia. The mean MMSE score was 27.17 ± 2.64, and the mean MoCA score was 22.53 ± 3.91. RESULTS: The sample consisted of 30 Afrikaans-speaking outpatients with schizophrenia. The MMSE and MoCA scores for each participant were matched and compared using the non-parametric Wilcoxon matched pairs test.
Moca cognitive assessment versus other tests full#
Participants had at least seven years of formal education and had been in partial or full remission for at least 3 months.

METHOD: The Afrikaans versions of the MMSE and MoCA were administered to Afrikaans-speaking adult outpatients. The objective of this study was to compare the results of the MMSE and MoCA in a group of outpatient schizophrenia sufferers to contribute to research into the instruments' potential usefulness as screening tools for cognitive impairment in schizophrenia. Nevertheless, the Montreal Cognitive Assessment Test (MoCA) and the Mini-Mental State Examination (MMSE) show promise in this regard. Unfortunately there are no validated, brief screening instruments for the detection of cognitive impairment in schizophrenia. In most clinical settings comprehensive neuropsychological testing to detect cognitive impairment in schizophrenia patients is not readily available, but because cognitive deficits in schizophrenia are clinically important it would be useful to detect or at least screen for them in a clinical setting. This better discrimination was more evident in the more educated group.Īddenbrooke’s Cognitive Examination Alzheimer disease Memory Impairment Screen Mini-Mental State Examination Montreal Cognitive Assessment Neuropsychological assessment Rowland Universal Dementia Assessment Scale Screening.A comparison between the Mini-Mental State Examination and the Montreal Cognitive Assessment Test in schizophreniaĭepartment of Psychiatry, School of Medicine, University of Pretoria, South AfricaīACKGROUND: Cognitive impairment is a core feature of schizophrenia that also has strong prognostic significance. The ACE-III achieved the highest diagnostic accuracy. Implementing normative data improved the diagnostic accuracy of the ACE-III but not that of the other tests. All tests, especially the ACE-III, conveyed a higher diagnostic accuracy in patients with full primary education than in the less educated group. Memory scores of the ACE-III and of the RUDAS showed a better diagnostic accuracy than those of the MMSE and of the MoCA. The Mini-ACE score from the ACE-III showed the highest diagnostic capacity (area under the curve 0.939).

The area under the curve was 0.897 for the ACE-III, 0.889 for the RUDAS, 0.874 for the MMSE, 0.866 for the MIS, and 0.856 for the MoCA.
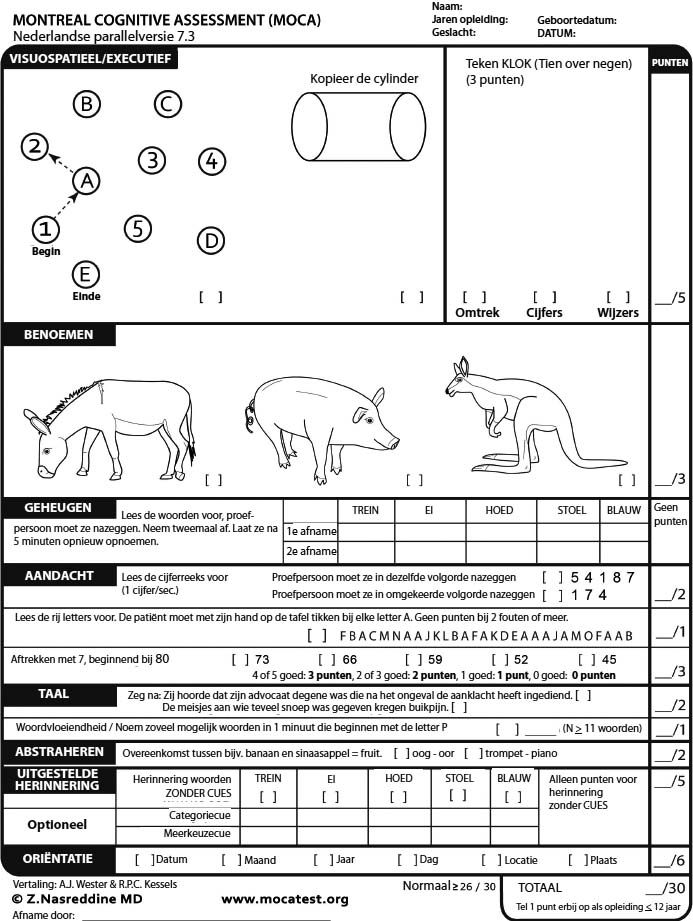
The diagnostic properties of the following tests were compared: Mini-Mental State Examination (MMSE), Addenbrooke's Cognitive Examination III (ACE-III), Memory Impairment Screen (MIS), Montreal Cognitive Assessment (MoCA), and Rowland Universal Dementia Assessment Scale (RUDAS).Īll tests yielded high diagnostic accuracy, with the ACE-III achieving the best diagnostic properties. We conducted a prospective and cross-sectional study of 92 patients with mild AD and of 68 healthy controls from our Department of Neurology. Our aim was to evaluate and compare the diagnostic properties of 5 screening tests for the diagnosis of mild Alzheimer disease (AD).


 0 kommentar(er)
0 kommentar(er)
